Products
Products
The importance of clinical bacterial culture:
According to a survey, the per capita annual consumption of antibiotics in China is about 138 grams, which is 10 times that of the United States and ranks first in the world. However, less than 20% of people truly need to use antibiotics, and over 80% of them belong to antibiotic abuse.
The abuse of antibiotics and other reasons lead to the infection of "super bacteria" in clinical practice, resulting in "no drugs available". According to statistics from the Ministry of Health, at least 80000 people in China die directly or indirectly from the abuse of antibiotics every year. The issue of antibiotic abuse has attracted high attention from national government departments and a series of effective measures have been taken.
The theme of World Health Day 2011 is "Resisting Drug Resistance: If you don't take action today, there will be no medicine available tomorrow". A document titled "Management Measures for Antibiotics in Medical Institutions" led by the Medical Affairs Department of the Ministry of Health of the People's Republic of China has been formed, which imposes the strictest regulations on the use of antibiotics in hospitals in terms of drug varieties, antibiotic product specifications, doctor prescriptions, and punishments. Hospitals and doctors who violate discipline and regulations will be subject to severe punishment measures such as demotion and cancellation of prescription rights.
Early microbial cultivation and targeted use of antibiotics for patient treatment based on the results of cultivation, identification, and drug sensitivity testing are important and necessary measures in clinical practice.
Regarding septicemia, bacteremia, sepsis:
General refers to a type of clinical syndrome caused by the invasion of pathogenic bacteria and their toxins into the bloodstream. During the course of the disease, inflammatory mediators are often activated and released, causing a series of clinical symptoms such as high fever, chills, tachycardia, shortness of breath, rashes, and changes in consciousness. In severe cases, it can cause shock, DIC, and multiple organ failure, with a high mortality rate.
Causes of the disease: Whether bacteria invading the human body can cause sepsis is closely related to the virulence, quantity, and immune defense function of the invading bacteria. Common reasons are as follows:
1. Skin and mucosal barrier damage: Damage and inflammation of the skin and mucosa, such as trauma and wound infection, extensive burns, open fractures, furuncles, carbuncle, infectious diarrhea, purulent peritonitis, etc., can easily be caused by bacteria entering the lymph or blood circulation from the damaged or inflamed area;
2. Various chronic diseases lead to the decline of immunity: malnutrition, blood diseases (especially those with leukopenia), nephrotic syndrome, cirrhosis, diabetes, malignant tumors, congenital reduction of immunoglobulin synthesis, and weakening of phagocytosis of white blood cells, which are easy to induce bacterial infection;
3. Clinical drug therapy: Various immunosuppressive drugs such as corticosteroids, antimetabolic drugs, anti-tumor drugs, and radiation therapy can weaken cellular or humoral immunity, and some can also reduce white blood cells or inhibit inflammatory reactions, which is beneficial for bacterial spread and diffusion.
4. Various examination or treatment measures: endoscopic examination, intubation examination, great saphenous vein intubation, indwelling catheter, venous hypernutrition therapy, various dialysis operations, organ transplantation, etc. can lead to bacteria entering the blood circulation, or infectious thrombosis and septicemia.
5. Abuse of antibiotics: it can easily lead to the proliferation of drug-resistant strains and increase the chances of infection;
6. 'Super bacteria': The variation of bacteria leads to changes in the spectrum of pathogenic bacteria;
Common clinical manifestations:
1. Symptoms of infection and poisoning: Most cases have a sudden onset, followed by chills or chills, followed by high fever, shock, etc.
2. Skin damage: characterized by ecchymosis, ecchymosis, and scarlatina like rash.
3. Gastrointestinal symptoms: often accompanied by vomiting, diarrhea, abdominal pain, and even vomiting and bloody stools.
4. Joint symptoms: joint swelling, pain, movement disorders, or joint effusion.
5. Hepatosplenomegaly: commonly seen in infants and young children, with mild or moderate enlargement; Some children may develop toxic hepatitis.
6. Other symptoms: severe cases are often accompanied by multiple organ failure symptoms such as myocarditis, endocarditis, heart failure, meningitis, pneumonia or lung abscess, confusion, lethargy, coma, oliguria or anuria, DIC, etc.
Common pathogenic bacteria:
Various microorganisms with pathogenicity or conditional pathogenicity can become pathogens of sepsis. Due to different ages, patients with different underlying diseases, different pathways of transmission and different age groups, the pathogenic bacteria are also different.
In the past, the main pathogens of sepsis were hemolytic streptococci and pneumococci, accounting for over 50% of the total, Staphylococcus aureus (Staphylococcus aureus+Staphylococcus aureus) accounting for 20%, and Gram negative bacteria accounting for about 12%. With the widespread application of broad-spectrum antibiotics, corticosteroids, and immunosuppressants, the spectrum of pathogenic bacteria for sepsis has also undergone changes.
In recent years, statistics show that Staphylococcus epidermidis and Staphylococcus aureus account for 40%~50% of the pathogenic bacteria, and anaerobes account for 8%~26% of the pathogenic bacteria of septicemia (many hospitals cannot do anaerobic bacteria detection). Most of them are bacteroides fragilis and Peptostreptococcus. Enterococcus and gram-negative bacilli account for 12%~23% of the infections. Fungal infections are on the rise, and the infection of multiple bacteria accounts for about 10%.
In addition to pathogenic bacteria with positive blood culture, the pathogenic infection of Sepsis with negative blood culture cannot be ignored.

Regarding blood culture (including sterile body fluid culture)
Blood culture (including sterile body fluid culture) is the simplest, most accurate and most commonly used method to detect blood and body fluid infections such as septicemia, bacteremia and fungemia, and is the etiological basis for identifying body blood and other infections.
Early aerobic and anaerobic blood culture and correct antibacterial treatment are the primary and necessary measures. Rapid and accurate isolation and identification of pathogenic bacteria based on cultivation results can provide extremely important information for diagnosis and treatment.
About Blood Bacteria (Fungi) Culture Bottles
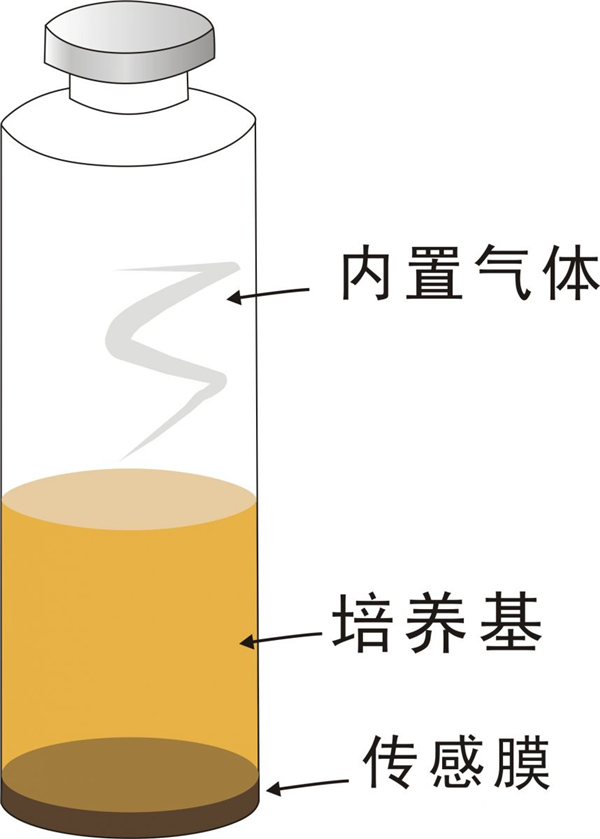
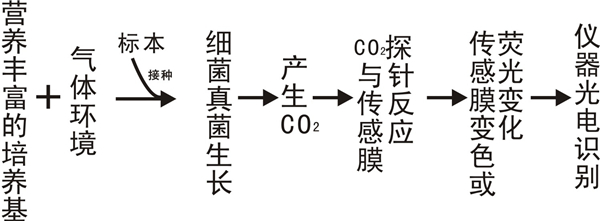
The blood bacteria (fungi) culture bottle (referred to as the blood culture bottle) is a highly sealed bottle with a built-in sensing membrane, culture medium, and gas environment that meets the needs of microbial growth.